#WeAreTogether: From dancing to prevent falls in older people to VR-based stroke rehab, patients in Berkshire are benefiting from a research partnership between the University and the NHS. Sarah Harrop reports on some of the projects.
Some of the biggest medical breakthroughs, such as proving the link between smoking and cancer, have been down to research carried out within the NHS – yet fewer clinicians than ever are managing to carve out time to do research because of pressures on the health service, according to a recent Academy of Medical Sciences report.
But Reading is helping to buck that trend, thanks to a productive partnership between the University and the Royal Berkshire Hospital NHS Foundation Trust.
Formed in 2017, the Collaborative Innovation Fund has funded more than 30 research, teaching and training projects to trial some innovative new ideas to improve patient care. Here we take a look at some of them.
Why is heart disease more common in diabetics?

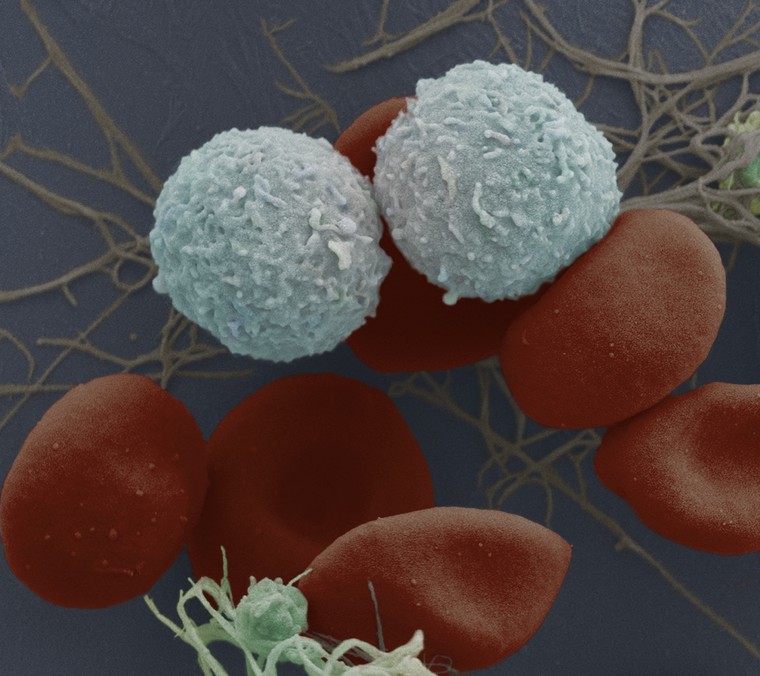
Platelets are blood cells that are involved in blood clotting. People with diabetes have a higher risk of getting heart disease than healthy people, and research suggests that platelets play a part in this by triggering unwanted blood clotting in the heart (thrombosis) – but it’s not yet known why this is.
One reason could be that not everyone’s platelets are the same. A team led by Professor Jon Gibbins from the School of Biological Sciences and Charlie McKenna, Consultant Cardiologist at the Royal Berkshire Hospital, is working on grouping patients with heart disease and diabetes by the particular characteristics of their platelets (their phenotypes).
The research project will run tests on patients’ blood samples and then use machine learning to allocate people to different phenotype groups. The first patient was recruited to the study in January 2020.
Virtual stroke rehab to boost confidence
People who have had a stroke can lose the ability to move their limbs or can only manage jerking, clumsy movements. They need to spend many months in rehabilitation to fully regain control of their arms and legs – which can be frustrating and emotionally exhausting.
Dr Yoshi Hayashi from the School of Biological Sciences is investigating the use of Virtual Reality to speed up and improve rehabilitation of upper limb control in these patients.
Wearing a VR headset, patients will be asked to pick up a virtual cup from a virtual table. Unlike the real life situation, the idea is that VR simulates perfect body motion and gives the user the experience of successfully reaching the cup. This feeling of agency gives the patient encouragement and the research team want to discover if this could help speed up their rehabilitation.
Mind over matter
Around one third of women who undergo womb surgery called fibroid embolization find it extremely painful, while others find their pain can be controlled with drugs and are in and out of hospital in a day.
Consultant radiologist Mark W Little and Dr Richard Harrison, postdoctoral researcher in pain at the University’s Centre for Neuroscience and Neurodynamics, are leading a study to predict which women will be vulnerable or more sensitive to pain.
Sleep, anxiety, depression and worrying about pain are known to predict the levels of actual pain experienced. The team have developed a two-page psychometric test for patients designed to predict a woman’s risk of suffering extreme pain following fibroid embolization. This could prove a simple but effective way to avoid painful experiences for these women as well as reducing the cost to the NHS of overnight stays.
The study is due to report its findings in June 2020.
Personalised medicine for people with diabetes
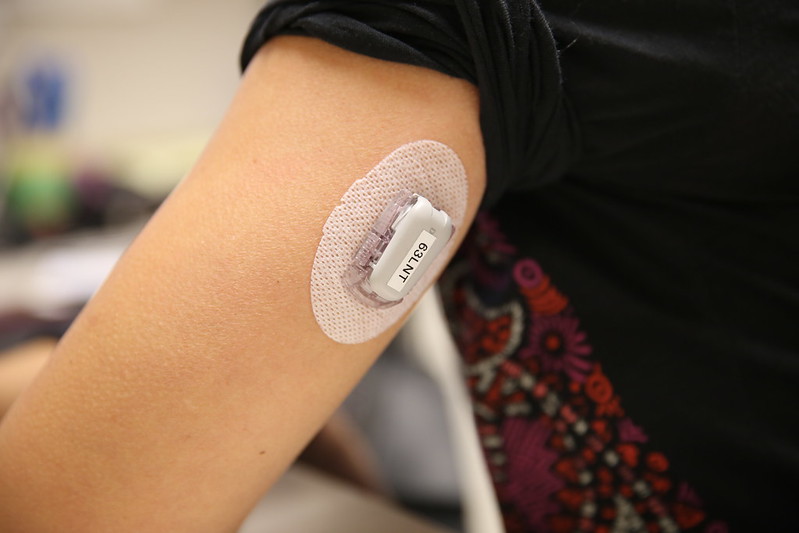
Diabetes is an increasing problem across the world, affecting nearly 4 million people in the UK alone. People with the disease have too much sugar in their blood because they can’t produce enough of the hormone insulin, which keeps blood sugar levels steady.
Dr Vicky Li is leading research to develop personalised treatments for those diabetes patients who are at higher risk of having dangerous swings in their blood sugar levels, helping them to see off spikes in blood sugar before they happen.
Working with 100 patients at the Royal Berkshire Hospital, the team used data from continuous glucose monitors – a sugar sensor that sits under the skin – to pick out those individuals who are at risk of spikes in glucose levels. They also looked at the amount of exercise patients did and their dietary intake of carbohydrates. Patients were then grouped according to their patterns of blood sugar variability.
By grouping people according to their individual characteristics and collecting their data, computerised models can be ‘trained’ to predict a patient’s peaks and troughs in blood glucose over time so that they can judge the amount of insulin they will need to inject more accurately. It will also help to design bespoke diets for this group of patients that keeps blood sugar levels steady, and a more tailored treatment approach.
In future, the computer model that predicts glucose variability could be developed into a ‘closed loop’ insulin pump which automatically adjusts the amount of insulin required. This could give patients a far better quality of life, for example they would be able to get a full night’s sleep without having to wake and take their insulin.
Results from the study show that the team’s deep learning model can predict blood glucose an hour ahead with higher prediction and clinical accuracy than existing methods. It shows promise for supporting patients with type 1 diabetes to better manage their behaviour to prevent dangerous spikes in blood sugar.
Clearer information for patients before they go under the knife

Knowing the risks of treatments they are about to undergo is essential for NHS patients to help them make informed decisions about their care and has been a requirement since the 1950s, yet many patients still go into procedures without a clear understanding of the risks involved.
Typography Professor Alison Black has carried out research with a charity and the Royal Berkshire Hospital to design clearer information materials for patients with so-called ‘difficult airways’ – airways that are damaged or diseased and therefore cannot tolerate the ventilation tubes usually used in surgery.
The team has developed publications to support consultations before surgery, and explain emergency anaesthetic procedures that doctors carry out in patients with difficult airways. This could help anaesthetists in framing how they speak to patients and gives patients a much clearer idea of the risks involved and the significance of those risks to them.
Visualising blood vessel damage
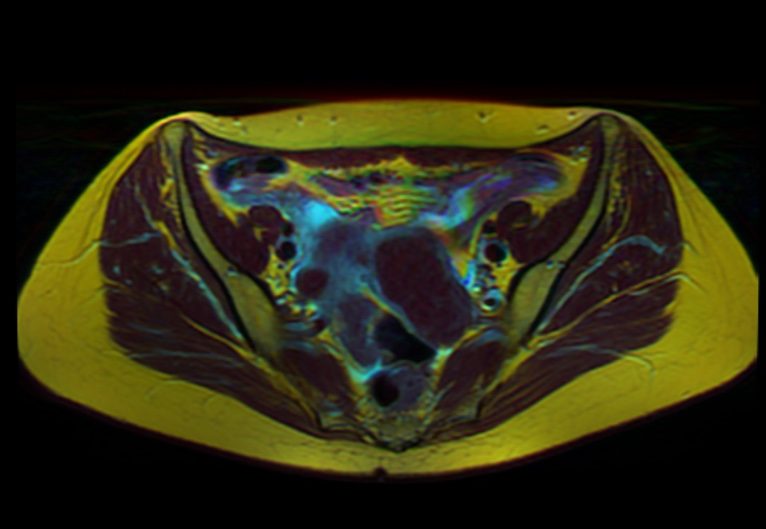
Research to better visualise blood vessel damage in kidney disease patients could help clinicians better understand why some go on to develop blockages or narrowing of blood vessels and how it happens.
Narrowed blood vessels (stenoses) are often seen in patients with kidney disease who need regular dialysis to clean their blood. This involves connecting one of their arteries to a vein, so the vein expands under pressure (known as a fistula) and can have a needle inserted to run blood through the dialysis machine.
The narrowing is thought to be caused by high pressure and irregularities in blood flow through the vessels and the body attempting to heal damage from fast flowing blood. Up to 75% of fistulas end up needing surgery or stretching with a balloon to clear the blockage within the first year of treatment – at a cost to the NHS and adding to the discomfort and time in hospital for patients.
A team led by RBH radiologist Farhan Ahmad and involving Dr Richard Harrison from the University’s Centre for Intergrative Neuroscience and Neurodynamics (CINN), created 3D models of the blood vessels in the arms of three healthy volunteers using ultrasound and Magnetic Resonance Imaging (MRI) to take pictures of veins and arteries.
They wanted to discover if ultrasound could be used to produce accurate 3D models of blood vessels to monitor blood flow in diabetes patients with fistulas. The advantage of ultrasound is that it is far cheaper and more widely available than MRI.
Working with Dr Yongmann Chung and computational modellers at the University of Warwick, the team applied dynamic fluid modelling to the images, to simulate the flow of blood through the vessel. Early results are highly promising. These models offer an exciting new avenue to help predict who is at risk of complications emerging from their fistulas.
The research could help clinicians better understand why some patients go on to develop blockages or narrowing of the veins and how it happens. It will also support an application to the National Institute for Health Research (NIHR) – the research arm of the NHS – to study fistulas in dialysis patients over time.
Dancing away risk of falls

Falls in elderly people are common and can cause injuries from which a frail older person will never fully recover. They also cost the NHS around £2.3 billion every year.
Margot Gosney, Professor of Geriatric Medicine, and Juliane Honisch in the School of Psychology and Clinical Language Sciences are leading a project to discover whether regular dancing can improve balance and reduce risk of falls in this group, and which types of dance might be effective. Dancing the tango, for example, may be more effective than the waltz for improving balance.
The study is currently recruiting over 50 patients who will take part in either conventional exercise programmes or regular dance classes with a partner. If successful, the research findings could provide the evidence for a low cost, simple and enjoyable way to reduce the risk of falls. Result are expected in October 2020.
Find out more about the University of Reading’s health research partnership with the Royal Berkshire Hospital NHS Trust on our website.
