For World Antimicrobial Awareness Week, Jessica Hayward, a Research Associate in Pharmaceutics at the University of Reading, explains about her work on a project developing miniaturised rapid antimicrobial testing.
Having always had a keen interest in medical microbiology, I joined the University of Reading after seeing a research post advertised that was focusing on developing a miniaturised rapid antibiotic susceptibility testing device to help select effective antibiotic therapy to treat patients with a bacterial infection (such as a UTI).

The role interested me having worked as a Specialist Biomedical Scientist in Microbiology for the NHS and also as a Production/Quality Control Scientist for a company which developed and manufactured diagnostic products for clinical and food laboratories. Although working in the NHS and industry were very different, my roles have always involved working towards improving patient care and supporting healthcare providers. I had been fortunate to be able to use some more modern identification/antibiotic susceptibility systems while working at the NHS, so I was excited to have the opportunity to get involved with developing a novel point-of-care test.
What is antimicrobial resistance (AMR)?
Antimicrobial resistance happens when microorganisms evolve and are no longer susceptible to the antibiotics used to treat infections. There is also potential for genes coding for antibiotic resistance to be spread between organism populations, increasing the spread of disease caused by resistant organisms. These organisms can cause serious illnesses that can become very difficult to treat and as a result, antimicrobials which are usually classed as “the last line of defence” may have to be used to treat the infection.
As the resistant population spreads, these specialist antibiotics become more commonly used, therefore increasing exposure to the microorganism population and eventually resulting in resistance against the “last resort” antibiotics. Given that most resistant microorganisms are more prevalent in clinical settings than in the community, this poses a huge risk to patients who are already receiving medical care. Antimicrobial resistance leads to increased hospital stay length, medical costs, and mortality rates.
Diagnosing AMR
Diagnosis of infection needs to be rapid to have successful patient outcomes, particularly when diagnosing and treating urinary tract infections (UTIs). Looking at just urine samples alone, more than 300 urines are processed each day in an NHS laboratory, and often many more in larger hospital laboratories.
For many laboratories in the NHS, it is still standard practice to use disc susceptibility tests, E tests and Vitek 2 (or similar automated antimicrobial susceptibility test devices) to determine whether a bacteria is sensitive (killed) or resistant (not killed) to a range of antibiotics. Rapid tests are available, such as PCR test kits, which can detect antimicrobial resistance mechanisms as fast as within an hour, directly from the sample without the need for a prior culture of the organism. However, these kits are expensive and are used to target specific, known resistance genes (for example carbapenemase-producing genes) as opposed to detecting a larger antibiotic profile of the causative organism.
How will our research project impact AMR?
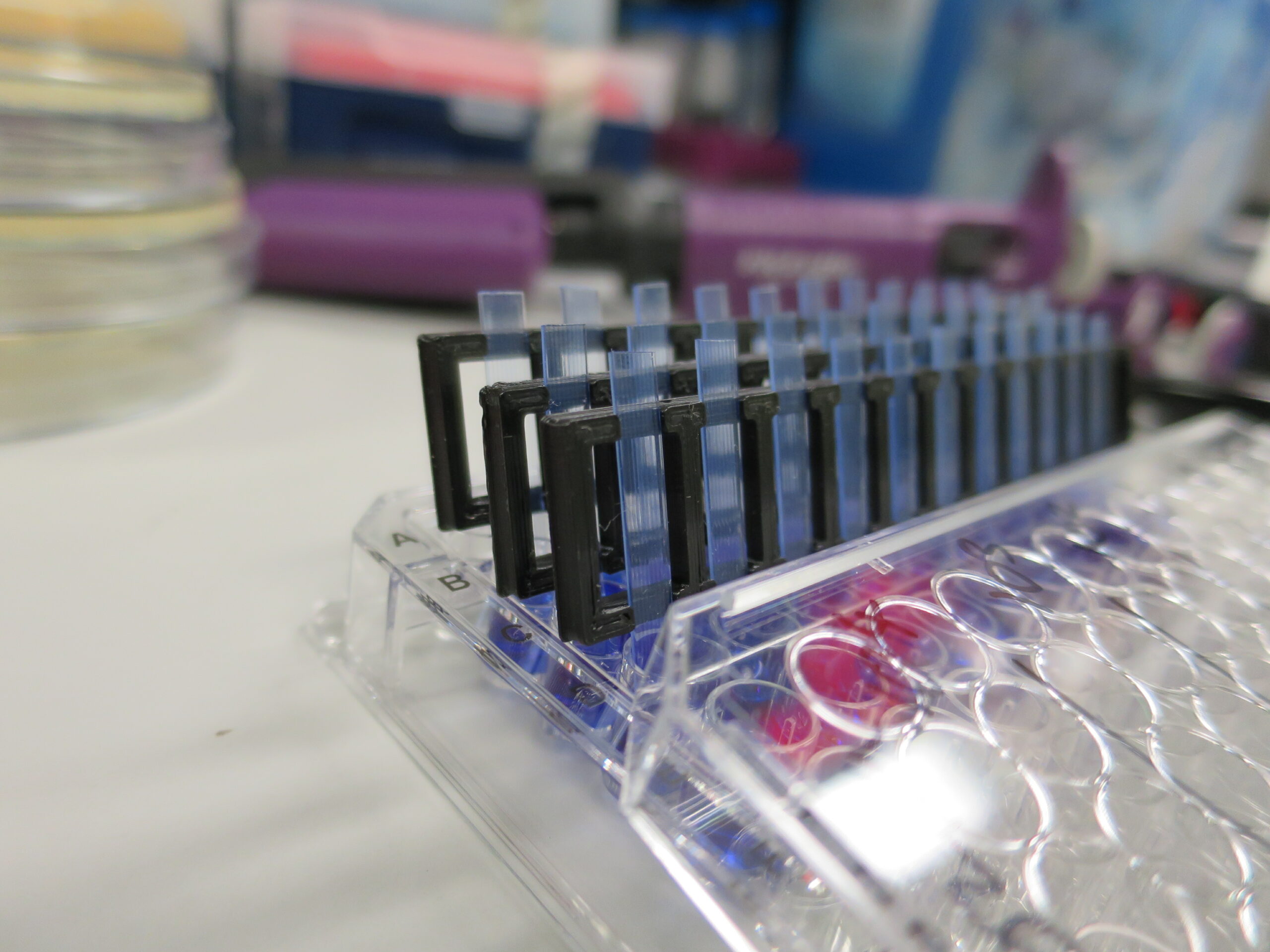
Our research uses microcapillary technology to miniaturise traditional microbiology tests (such as broth microdilution) to analyse tiny volumes of samples (such as urine) without the need to culture the specimen prior to testing (as is required with conventional methods).
The test device uses low-cost mass-manufactured microcapillary film which will offer high throughput testing using a portable device, allowing for testing outside of the laboratory. This will lead to much faster results which can be used to support healthcare providers to tailor the treatment for a patient rather than treating it blind.
Administering the correct and most effective antibiotic will help to limit antibiotic treatment failure, reduce the emergence of further antimicrobial resistance and prevent long hospital stays. Informing clinicians of the most effective antibiotic to treat the infection will also help to prevent antibiotic overuse which is a major risk factor for Clostridium difficile infection.
Microbiological testing of samples is important and there will still be a need to culture organisms to test for extended antimicrobial susceptibility and accurate organism identification. However, novel rapid antimicrobial testing can give a much quicker insight into whether the proposed empiric therapy is likely to be effective or not before treatment has even been administered to the patient.
Read more about Microfluidic Antimicrobial Resistance Tests.